Strategically Accelerate COVID-19 Diagnostics from Development to Market – Webinar Summary
On June 11, 2020, a panel of experts from Precision for Medicine discussed approaches to Strategically Accelerate COVID-19 Diagnostics from Development to Market, available to watch on demand. The conversation covered approaches for accelerating the development of diagnostics for COVID-19, including building a biospecimen foundation for product development, navigating the regulatory landscape for serology tests, and leveraging important design considerations for market access.
Panel experts included:
- Jim Boushell, Vice President, Biospecimens Solutions
- Karen Richards, Senior Vice President, In Vitro Diagnostics and Quality
- David Parker, Senior Vice President, Diagnostics Solutions
Since the emergence of COVID-19, many diagnostic and therapeutic developers have pivoted their programs to COVID-19. Many of these programs have been delayed or derailed because of unforeseen challenges. In this webinar, the panel explored real-world examples from their participation in multiple COVID-19 research studies to help diagnostic developers anticipate pitfalls, mitigate risk, and accelerate development.
The panel began with an overview of potential development challenges, including vetting biospecimen sources to mitigate downstream risk, effectively planning for post-EUA times and the FDA 510(k) process, and developing assays that fit within an evolving payment landscape.
Contact us today
Sourcing biospecimens
Jim Boushell discussed the critical importance of biospecimens in discovery, development, and diagnosis, and explained how the COVID-19 pandemic has disrupted the traditional supply of biospecimens.
Boushell explained, “Having a long-term collection program with timed sampling of patients who have consented to additional testing provides insights that enable researchers to map the pathway from immune cell receptors to specific SAR-CoV-2 antigens. These insights would be valuable for understanding response to treatment or developing more specific diagnostic tests.”
Boushell emphasized the value in being able to interrogate large cohorts of treatment-naive samples, which would be difficult—if not impossible—to replicate a year from now. He also discussed the importance of having access to large cohorts of diagnosed, at-risk, and clinically healthy samples for challenging and understanding assay performance. He then shared a patient-centric process that Precision for Medicine originally developed to build rare disease biorepositories and is now leveraging to support the development of COVID-19 diagnostics.
A successful biospecimen plan is proactively designed to support a specific diagnostic program. Boushell provided tips for developing a biospecimen plan, beginning with documenting an endpoint to guide cohort selection and then aligning with a partner that has the resources to not only source, supply, and manage biospecimens, but also the infrastructure to support downstream capabilities such as stratification, outcomes investigations, and future research endpoints.
 Jim Boushell
Jim BoushellVice President,
Biospecimens Solutions
Planning for post-EUA times and the FDA 510(k) process
Karen Richards continued the conversation with an overview of 3 pathways for EUA of serological tests for SARS-CoV-2 antibodies. Although each of these pathways has its nuances, all of them require that the test be analytically validated, that a clinical agreement study is performed, and that the product is labeled properly. Richards also covered the key studies required for analytical validation and clinical agreement.
For developers planning for a post-EUA submission for marketing authorization, Richards provided this advice regarding timing of the EUA, “Balance the risks of being first-to-market under EUA and subject to changes to policy requirements or additional data to support a future marketing claim with the benefit of setting the standard for requirements other manufacturers will need to follow.”
Richards also stressed the importance of managing an EUA with a future FDA submission in mind. Factors to consider include the analytical studies and sample types needed, as well as the regulatory requirements. For those considering a future marketing submission to the FDA, it may be worthwhile to test as many natural specimens as possible for EUA that can be leveraged later for de novo or 510(k) submission. Early communications with the agency now might also accelerate guidance to support clearance for serology devices over the next year, lowering the barrier to market entry.
 Karen Richards
Karen RichardsSenior Vice President,
In Vitro Diagnostics and Quality
Assays that fit within an evolving payment landscape
David Parker followed with a discussion on working within an evolving reimbursement environment. Market access and uptake of a diagnostic test depends on securing adequate reimbursement; and reimbursement is a function of coverage, coding, and payment. Parker pointed out that, for COVID-19 testing, coverage is provided by both Medicare and most commercial payers regardless of whether the test is authorized under EUA or traditional authorization pathways, though this may change when the supply of FDA-cleared tests can meet demand. It is also important to ensure that labs can afford to buy and perform the test within the available payment, as labor and fixed costs can consume 25% to 75% of the available reimbursement.
Parker then described the codes available for COVID-19 testing, including the codes for high-throughput tests performed on automated platforms that process more than 200 specimens per day and the codes for serology testing. He also provided details on payment rates. He cautioned listeners to be alert for reimbursement evolution, as the payments are currently at least 2.5 times greater than the parent code payment rates for methodologically similar tests and rates are likely to decrease over time.
Parker said, “Our perspective is that you can go to market with a relatively high cost and price structure, but it’s advisable that you work to reduce cost of goods as quickly as possible. When the public health emergency is declared to be over, and CMS prices the codes on the Clinical Lab Fee Schedule, you should expect reimbursement rates to drop until they are at or close to reimbursement for comparable traditional serology tests.”
COVID-19 diagnostic development requires overcoming a variety of obstacles, from sample sourcing and assay design to regulatory hurdles and reimbursement considerations. But, with a forward-thinking, long-term strategy that considers both the current and future state of the COVID-19 diagnostic landscape from sourcing to payment, developers can successfully navigate the path from EUA to market authorization and adoption.
 David Parker
David ParkerSenior Vice President,
Diagnostics Solutions
Precision for Medicine
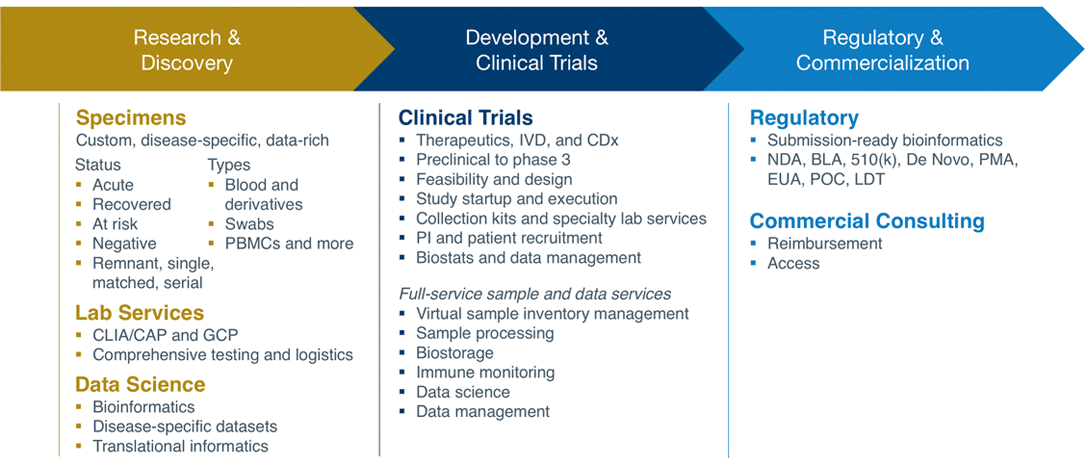
Precision for Medicine is an industry leader in the design, development, and execution of biomarker-informed clinical research and complex data management. Precision for Medicine is supporting the efforts of companies focused on developing COVID-19 diagnostics and therapeutics through its deep experience in respiratory and infectious diseases, regulatory expertise, biospecimen solutions, BSL-2 laboratories, biorepository, and comprehensive support for immune monitoring, antibodies, vaccines, and all related research.
Contact us today
Supporting the development of new treatments
Time-sensitive solutions to address COVID‑19
COVID‑19 Clinical Development Solutions
Biospecimens to Support COVID‑19 Research
Diagnostics and IVD Development Support
