The role of IHC in precision medicine
Immunohistochemistry (IHC) is a powerful tool that supports the identification of new ways to target complex diseases. It enables the exploration of diagnostic, predictive, and prognostic biomarkers, ultimately delivering precision medicine approaches that get the right treatment to the right patient at the right time. By enabling the visual detection of biomarkers in tissue sections, IHC can validate disease targets, assess biodistribution, detect off-target binding, inform patient enrollment in clinical trials, and determine treatment eligibility post-approval. The use of IHC leads to a deeper understanding of the mechanism of action and therapeutic potential of new treatments. It also supports better clinical trial design, enabling shorter clinical development timelines.
In this blog, we explore the journey from biomarker to clinical trial assay (CTA), highlighting the myriad applications of IHC in therapeutic development.
Beginning with the end in mind
In the context of personalized medicine, the end goal of IHC assay development is to provide an assay that can be used to guide a patient’s therapy. To that end, the IHC assay must be sensitive, specific, robust, and reproducible. It is also important to understand how the biomarker will be used, whether for risk categorization, diagnosis, prognosis, screening, or predicting response to treatment.
There are many factors that affect the performance of an IHC assay, from the time the sample is collected to the time that assay result is used to drive clinical decision-making. When developing an assay, it is critical to consider all the factors that may contribute to the success or failure of the test. The American Society of Clinical Oncology (ASCO) and the College of American Pathologists (CAP) have reported that up to 20% of all IHC assays worldwide may be inaccurate. These inaccuracies are largely attributable to pre-analytical factors such as cold ischemic time, the fixative used, and the time the sample remains in fixative. At Precision for Medicine, we provide biospecimens for use in IHC assay development and validation studies, including CAP-graduated formalin-fixed paraffin-embedded (FFPE) samples that have been processed according to current recommended guidelines.
Validating a biomarker
A good biomarker may either be overexpressed in disease or expressed in normal tissue but lost in disease. Since the completion of the Human Genome Project, there has been exponential growth in the number of newly recognized biomarkers. However, the development of accurate, reliable, and consistent immunoassays for these biomarkers has lagged.
Key factors in IHC assay development
Developing a reliable and reproducible IHC assay is critical for guiding clinical decision-making in precision medicine. Below are the essential considerations:
Antibody selection
With hundreds of vendors and over 400,000 primary antibodies for clinical and research use, a single target may have hundreds of available primary antibodies. Different antibodies to the same target can produce very different results. Antibody type, whether polyclonal, monoclonal, or recombinant, is an important consideration. Polyclonal antibodies are a heterogeneous mix of antibodies obtained by immunizing the species of interest. These antibodies tend to recognize multiple epitopes and are more sensitive, which can be advantageous for hard-to-detect targets. Monoclonal antibodies are derived from single B-cell clones. Recombinant antibodies are created using antibody-coated genes in high-yield expression vectors. Both monoclonal and recombinant antibodies offer greater batch-to-batch consistency than polyclonal antibodies but may require higher upfront development costs.
Among the commercially available antibodies, there are ready-to-use (RTU) and research-use only (RUO) antibodies. RTU antibodies require less validation overall because the vendor has already tested and validated the optimal dilution and provided a protocol. RUO antibodies are available as concentrates and will require initial optimization. This process, which can involve the use of positive and negative control cell lines and tissues to qualify the resulting antibody performance and assay conditions in the appropriate disease indication(s), is often best performed using tissue microarrays (TMAs).
Antigen retrieval method
Antigen retrieval is essential for unmasking antigens that have been cross-linked during tissue fixation. Methods like heat-induced epitope retrieval (HIER) use acidic or basic solutions to break down protein cross-links, ensuring accurate and reliable biomarker detection.
Species selection and cross-reactivity
The species from which an antibody is derived affects its specificity and cross-reactivity. It's important to control for cross-reactivity or non-specific binding through the use of isotype controls to ensure the accuracy of the assay.
Localization and staining patterns
Understanding expected antigen localization and staining patterns is key to interpreting IHC results. Websites like HumanProteinAtlas.org and literature reviews can provide valuable insights into these patterns.
Controls and test tissue
The key to finding the balance between signal and background is the use of appropriate controls. Positive control tissues express the biomarker of interest, ideally at low or intermediate levels, while negative controls are known not to express that biomarker. The negative control is also used to check for non-specific signals or false positives. Selecting proper controls can be difficult for new biomarkers, especially if there is little reference data concerning tissue expression. The best controls are usually cell lines with known expression levels of the biomarker of interest; however, these samples are relatively “clean”, with just the cells of interest present, so is it important to optimize antibody binding in tissue samples, where there will inevitably be more background staining to address.
Cut-off value/staining threshold
Defining cut-off values and staining thresholds is essential for correctly classifying tissue samples, especially when treatment decisions depend on the presence or absence of a biomarker.
Assay platform selection
At Precision for Medicine, we use all three major platforms—Dako, Leica, and Ventana. The choice of platform is typically based on client preference and the ultimate purpose of the assay.
Developing and optimizing an IHC assay
Success with IHC is underpinned by many factors. First and foremost are valid antibodies and thorough assay optimization prior to subsequent application. At Precision, we follow a standard approach when developing or optimizing a new IHC assay to achieve the desired sensitivity and specificity. We select two to three antibodies, perhaps from different vendors or different species, and evaluate three different concentrations with two different antigen retrieval times. Depending on performance of these initial studies, we may vary incubation times or change temperatures for antigen retrieval. In our laboratory, we tend to use FFPE samples because tissue architecture is maintained, and antibody distribution can be visualized in situ. However, the process of formalin fixation can affect the antigenicity of biomarkers via protein cross-linking, which may mask some of the antigens.
Antigen retrieval methods can be applied to overcome cross-linking and expose the target antigen. For example, heat-induced epitope retrieval uses slightly basic or acidic solutions to break down protein cross-links.
Applying IHC in preclinical and early clinical development
Validating disease targets and biomarkers
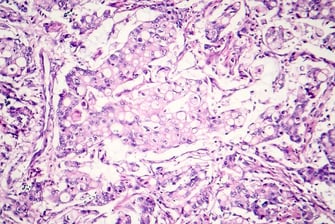
Preclinical analysis of human tissues enables understanding of target and biomarker expression in the population of interest and provides data to confirm, validate, or correlate with in vivo disease models. Target proteins can be interrogated across cohorts of diseased versus non-diseased controls to elucidate the localization and prevalence of expression (see Figure 1). These data can be used to narrow down the focus to specific disease indications.

Figure 1. Pyruvate kinase expression in lung cancer, where expression is cytoplasmic in healthy cells (yellow arrow) and nuclear in apoptotic cells (white arrow)
When it comes to understanding the potential range of target and biomarker expression in the proposed clinical trial population, and ultimately in the real world, the ability to interrogate large numbers of donors is critical. TMAs are useful in supporting preclinical target and biomarker prevalence studies since they provide a higher throughput approach where multiple donors can be evaluated within or across indications in a convenient format.
At Precision, we developed and validated a well-characterized TMA for investigating target and biomarker across the staged progression of Alzheimer’s disease. To achieve this, we sourced temporal cortex tissue from patients with early (Braak I and II), mid (Braak III and IV), and late (Braak V and VI) stage AD and selected test samples based on additional factors such as amyloid score, apolipoprotein E (APOE) genotype data, cerebrospinal fluid (CSF) pH, and clinical history. We then created a TMA comprising tissues from five individual donors per stage and five non-disease donors.
The resulting TMA was qualified using IHC for expression of hallmark disease markers: phosphorylated tau (p-tau) and amyloid beta (Aβ) 1-42, a hyperphosphorylated form of Aβ.

Figure 2. Qualification of TMA using IHC for expression of p-tau
Precision for Medicine further characterized the TMA by investigating two markers for microglia and astrocytes, both of which undergo changes in frequency and morphology in different stages of AD.
Another approach to validating targets or biomarkers is to evaluate relevant protein-protein interactions. Aberrant protein-protein interactions are associated with various conditions, including cancer, infectious diseases, and neurogenerative diseases. Targeting protein-protein interactions is an area for disease intervention and is an essential, albeit sometimes challenging, strategy for the development of new drugs. For instance, if the therapeutic approach is to disrupt a protein receptor interaction, an IHC-based proximity ligation assay can provide data on not just localization of the proteins within the tissues, but also their interactions.
Navinci has developed NaveniFlex for visualizing protein-protein interactions in tissues. This assay is designed to be used with primary antibody pairs, where each antibody is from a different species. Once the primary antibodies are bound, secondary Navenibodies, which are conjugated to oligonucleotide arms, bind to their respective primary antibodies. Only if Navenibodies are in proximity can they generate a DNA circle. Polymerase is then used to initiate a rolling circle DNA amplification. Finally, amplified DNA is detected using chromogenic or fluorescent probes to confirm localization and protein-protein interactions.
Assessing biodistribution of biotherapeutics
The disposition of an administered therapy is a key determinant of its efficacy. IHC assays can be developed to identify the presence of a biotherapeutic in tissue. These data can then identify which target organs the drug has reached or confirm that the drug has reached its intended location. While the analytical method used will depend on the type of biotherapeutic, the essence of the approach is using an anti-drug antibody to bind the biotherapeutic present within the tissue.
Detecting off-target binding
Many biotherapeutics are delivered intravenously into the systemic circulation and may come into contact with a plethora of tissue types. Thus, a critical assessment required by regulators as part of the Good Laboratory Practice (GLP) safety package is a tissue binding assay that evaluates the potential of the drug molecule to bind off-target. Of note, developing a tissue binding assay can be challenging, as biotherapeutics are often complex molecules. Further, the assay needs to be robust since the ideal scenario for this safety assessment assay is to see a negative result—and that negative result needs to be truly negative, not just a consequence of an unsuitable assay.
Using IHC in early clinical development
Supporting patient enrollment
To support enrollment in a global Phase 1 oncology study, Precision developed and validated a custom IHC assay, reagent kit, and scoring index (SI) for assessing P-cadherin, a cellular adhesion protein that contributes to oncogenesis. The SI was based on the tumor area stained multiplied by the staining intensity (see Figure 3). This assay was rolled out to three global clinical sites, and study eligibility required an SI of 4 or higher for enrollment. Patients whose tumor biopsies had an SI of 4 or higher were eligible for enrollment.

Figure 3. Development of a custom IHC assay and scoring index for enrollment into a Phase 1 study
Each site ran the IHC assays independently and used their own pathologists to do the analysis. Precision served as the central lab, performing independent mass analysis of site results and finding almost a 92% concordance in the results. This demonstrates the feasibility of developing and fully validating an IHC assay at a single center and then running that assay at multiple sites across the globe to support patient selection.
Integrating IHC with digital pathology and AI
With the volume of pathology work required to support target and biomarker discovery and assay validation, keeping track of all the data generated and having a robust audit trail is crucial. At Precision, we use HALO AP from Indica Labs to manage our pathology images, data and clinical trial workflow. With a significant biorepository of FFPE tissue samples with well-curated pathology data sets, the slide images (H&E, IHC, special stains) and associated data (pathology, clinical, NGS) are highly sought after for training artificial intelligence (AI) and machine learning. Our digital images, along with our pathologist- and oncologist-supported scoring and interpretations, can be used as training sets for machine learning algorithms that have the potential to detect new targets and biomarkers, automating discovery and moving it into the cloud.
Conclusion
Successful application of IHC is dependent upon reliable and robust antibodies, scientifically rigorous methods, access to quality samples, and a talented team of scientists. At Precision, we support preclinical target and biomarker validation, biotherapeutic disposition and safety, and clinical development from first-in-human trials all the way to market with exploratory biomarker assays, clinical trial assays, and companion diagnostics. We combine years of experience and expertise in delivering IHC assay data, with our ability to support the entire development process, from custom kitting for clinical sites to sample management logistics, histopathology, and centralized pathology capabilities that allow for rapid data turnaround for enrollment decisions.
Learn more about Precision's immunohistochemistry (IHC) services>
We also recommend:
Watch our on-demand webinar to learn about the foundational laws and standards, aligning your IHC validation and regulatory strategies with US clinical trial goals, and understanding regulatory differences between the US and Europe.